


Afterward, vitamin D 3 is metabolized in the liver to 25‐hydroxyvitamin D (calcifediol or calcidiol 25OHD 3 or 25(OH)D), a reliable marker of vitamin D status. In the skin, solar ultraviolet‐B radiation converts 7‐dehydrocholesterol to previtamin D 3, which is then rapidly converted to vitamin D 3. Vitamin D can be obtained from food, dietary supplements, or synthesized in response to sunlight. ) However, prevalence rates for this condition vary depending on the defined thresholds, because there is no consensus on optimal concentrations, not even for its principal effect on skeletal tissue, for which the benefits of vitamin D have been clearly demonstrated.

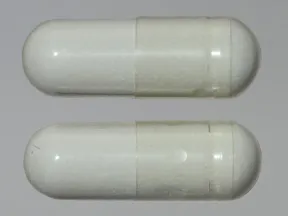
Vitamin D deficiency is a worldwide public health issue affecting more than one billion people. Journal of Bone and Mineral Research published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research (ASBMR). These results thus confirm that calcifediol is effective, faster, and more potent than cholecalciferol in raising serum 25(OH)D levels and is a valuable option for the treatment of vitamin D deficiency. No relevant treatment‐related safety issues were reported in any of the groups studied. The most remarkable difference between both drugs in terms of mean change in serum 25(OH)D levels was observed after the first month of treatment (mean ± standard deviation change = 9.7 ± 6.7 and 5.1 ± 3.5 ng/ml in patients treated with calcifediol and cholecalciferol, respectively). At month 4, 35.0% of postmenopausal women treated with calcifediol and 8.2% of those treated with cholecalciferol reached serum 25(OH)D levels above 30 ng/ml ( p < 0.0001). Patients with baseline levels of serum 25(OH)D <20 ng/ml were randomized 1:1:1 to calcifediol 0.266 mg/month for 12 months, calcifediol 0.266 mg/month for 4 months followed by placebo for 8 months, and cholecalciferol 25,000 IU/month for 12 months. A total of 303 patients were enrolled, of whom 298 were included in the intention‐to‐treat (ITT) population. Results reported here are from a prespecified interim analysis, for the evaluation of the study's primary endpoint: the percentage of patients with serum 25‐hydroxyvitamin D (25(OH)D) levels above 30 ng/ml after 4 months. This 1‐year, phase III–IV, double‐blind, randomized, controlled, multicenter clinical trial assessed the efficacy and safety of calcifediol 0.266 mg soft capsules in vitamin D–deficient postmenopausal women, compared to cholecalciferol. Few supplementation guidelines mention calcifediol treatment, despite being the direct precursor of calcitriol and the biomarker of vitamin D status. Furthermore, vitamin D deficiency has become a worldwide health issue. Vitamin D has shown to play a role in multiple diseases due to its skeletal and extraskeletal actions.


 0 kommentar(er)
0 kommentar(er)
